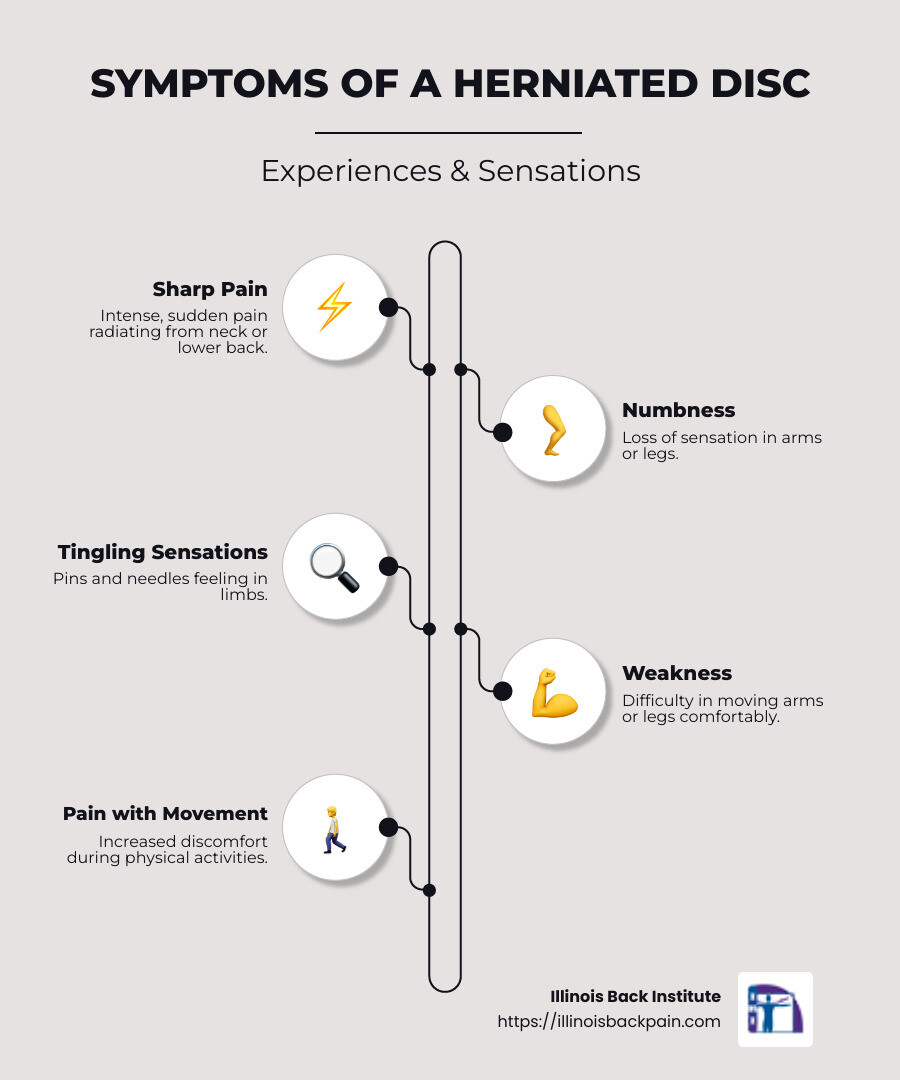
What does a herniated disc feel like? If you’ve ever experienced sharp, shooting pain down your arm or leg, you might already have a clue. A herniated disc, often known as a slipped or ruptured disc, can cause severe discomfort that radiates from your neck or lower back into other parts of your body. Symptoms can include:
- Sharp, burning, or shooting pain
- Numbness or tingling sensations
- Feelings of weakness in your limbs
- Pain that gets worse with movement
Back pain is a common issue that affects millions, but not all back pain is created equal. Understanding the nuances of what a herniated disc feels like can help in seeking the right treatment. Imagine carrying a heavy backpack day after day; eventually, it weighs on you. Your spine works similarly, bearing the brunt of life’s everyday stresses.
A herniated disc happens when the soft material inside a spinal disc bulges out, pressing on nearby nerves. This can result in pain, weakness, and even changes in sensation, making daily activities difficult. The good news? With Functional Disc Stabilization™, you can find relief without surgery or medications, regaining your mobility and comfort.
Understanding Herniated Discs
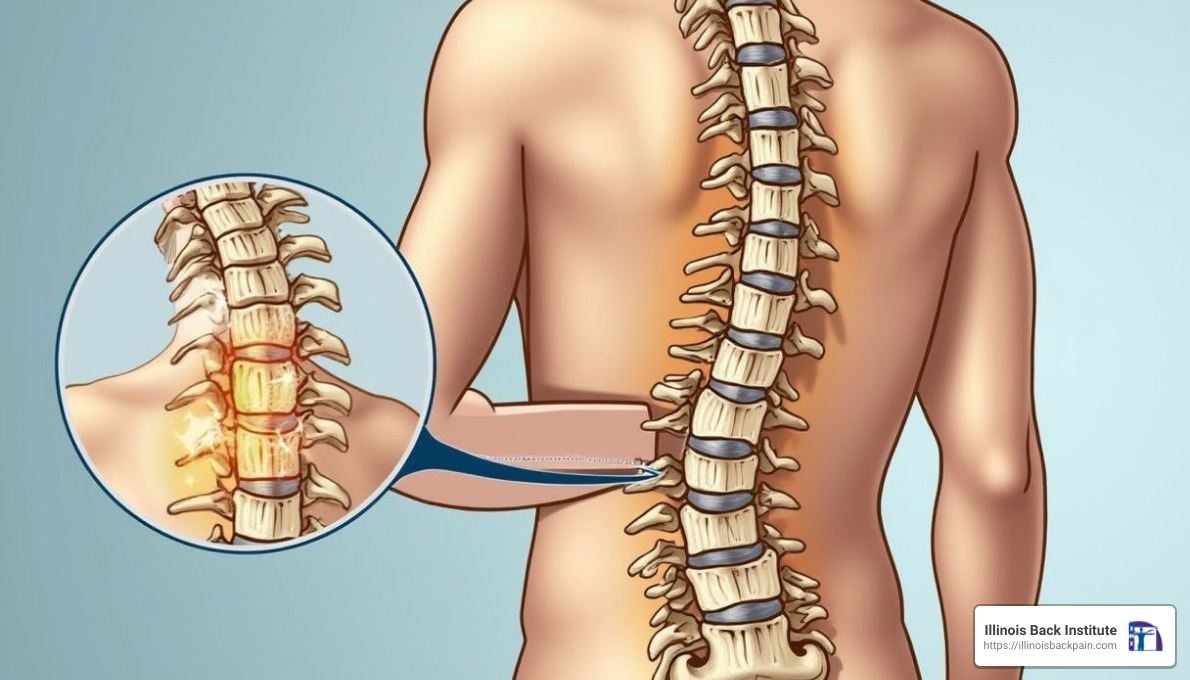
Your spine is like a stack of building blocks, where each block represents a vertebra. Between these vertebrae are small, cushion-like discs that act as shock absorbers. These discs allow your spine to bend and twist smoothly.
The Structure of a Spinal Disc:
- Nucleus Pulposus: This is the jelly-like center of the disc. Think of it as the soft, squishy center of a jelly donut. It provides the disc with its cushioning ability.
- Annulus Fibrosus: Surrounding the nucleus pulposus is a tough, rubbery outer layer. This layer keeps the nucleus contained and protects the spinal cord.
A herniated disc occurs when the nucleus pulposus pushes through a tear in the annulus fibrosus. This can happen due to sudden injury or gradual wear and tear. When the nucleus leaks out, it can press on nearby nerves, causing pain and other symptoms.
Why Does This Happen?
- Age: As we age, discs naturally lose some of their water content, becoming less flexible and more prone to tearing.
- Injury: Lifting something heavy or twisting awkwardly can cause a disc to herniate.
- Repetitive Strain: Repeated movements that stress the spine can also contribute to disc damage over time.
Understanding the anatomy of a herniated disc helps explain why it causes pain. When the nucleus pulposus escapes, it irritates nearby nerves, leading to symptoms like sharp pain, numbness, and tingling.
Fortunately, non-surgical treatments like Functional Disc Stabilization™ can offer relief. This innovative approach is non-invasive, drug-free, and has helped countless patients regain their strength and mobility. It reverses disc degeneration, providing a healthier back without the need for surgery or medications.
In the next section, we’ll dig into what a herniated disc actually feels like and how it affects different parts of the spine.
What Does a Herniated Disc Feel Like?
A herniated disc can be a real pain—literally. When the jelly-like center of a spinal disc pushes through the tough outer layer, it can press on nearby nerves, causing a range of uncomfortable symptoms. Let’s break down what a herniated disc feels like and how the symptoms vary depending on its location in the spine.
Symptoms by Location
Lumbar Spine (Lower Back)
- Sharp Pain: Often described as a shooting pain, it can start in the lower back and travel down the leg, sometimes reaching the foot. This is because the herniation can press on the sciatic nerve, leading to a condition known as sciatica.
- Numbness and Tingling: You might feel these sensations in the buttocks, thigh, calf, or foot.
- Weakness: Some people experience muscle weakness, making it hard to lift the foot (a condition known as “foot drop”).
Cervical Spine (Neck)
- Sharp Pain: Pain may radiate from the neck to the shoulder blade, arm, or hand. It can feel like an electric shock.
- Numbness and Tingling: These sensations often occur in the shoulder, arm, or hand.
- Weakness: This might affect your ability to grip objects or perform fine motor tasks like writing.
Common Misdiagnoses
Herniated discs can mimic other conditions, which can lead to misdiagnoses. Here are a few common ones:
- Piriformis Syndrome: This condition causes sciatic nerve irritation, similar to a herniated disc in the lumbar spine. However, the pain originates from the piriformis muscle in the buttocks.
- Sciatica: While sciatica is a symptom of a herniated disc, it can also arise from other issues like spinal stenosis or a bone spur.
- Osteoarthritis: This degenerative joint disease can cause similar symptoms, such as pain and stiffness, making it sometimes difficult to distinguish from a herniated disc.
Understanding these symptoms and potential misdiagnoses is crucial for getting the right treatment. If you suspect a herniated disc, it’s important to consult with a healthcare provider who can perform a thorough examination and recommend the best course of action.
In the next section, we’ll explore how healthcare professionals diagnose a herniated disc and what you can do to assess your symptoms at home.
Diagnosing a Herniated Disc
When it comes to figuring out if you have a herniated disc, a combination of professional evaluations and self-assessment techniques can help. Here’s how healthcare professionals and you can work together to get a clear diagnosis.
Professional Evaluation
Physical Exam
Doctors typically start with a physical exam. They’ll ask about your medical history and symptoms. You might be asked to lie flat, move your legs, or perform other simple movements to check for pain and mobility issues. They’ll also test your reflexes and muscle strength to see if any nerves are affected.
Imaging Tests
If a physical exam suggests a herniated disc, imaging tests can confirm it:
- MRI (Magnetic Resonance Imaging): This is the most common test for diagnosing herniated discs. It provides detailed images of the spine, helping to pinpoint the location and severity of the herniation.
- CT Scan (Computed Tomography): Sometimes used if MRI isn’t available, a CT scan offers a good view of the spinal structures.
- EMG (Electromyography): This test measures the electrical activity of muscles and can help determine if a nerve is being compressed by a herniated disc.
Self-Assessment Techniques
While professional evaluations are crucial, there are ways you can assess your symptoms at home:
Bending Movements
Pay attention to how your body reacts to certain movements. Does bending forward or backward trigger pain? Does the pain radiate down your leg or arm? These could be signs of a herniated disc.
Pain Assessment
Rate your pain on a scale from 1 to 10. Note when the pain worsens or eases. Does it get worse with specific activities like sitting, standing, or walking? Keeping a pain diary can help your doctor understand your condition better.
Next Steps
Identifying a herniated disc early can lead to more effective treatment options. The Illinois Back Institute offers Functional Disc Stabilization™, a non-invasive, non-surgical, and drug-free treatment that has helped tens of thousands of patients. This approach focuses on reversing disc degeneration, providing a healthier and stronger back without the need for medications or surgery.
In the next section, we’ll dive into the various non-surgical treatment options available for managing herniated disc symptoms.
Non-Surgical Treatment Options
Living with a herniated disc can be tough, but there are several non-surgical treatments that can help you find relief. Let’s explore some of these options.
Rest and Activity Modification
Taking it easy is often the first step in managing a herniated disc. Resting for a few days can help reduce inflammation and relieve pain. However, it’s crucial not to overdo it. Too much rest can lead to muscle stiffness and weakness. Instead, aim for a balance between rest and gentle activity. Listen to your body and avoid movements that trigger pain.
Anti-Inflammatory Drugs
Over-the-counter anti-inflammatory medications, like ibuprofen or naproxen, can help reduce inflammation and alleviate pain. These medications can be effective for mild to moderate pain. Always follow the dosage instructions and consult your doctor if you’re unsure about what’s best for you.
Physical Therapy
Physical therapy is a cornerstone of non-surgical treatment for herniated discs. A skilled therapist can guide you through exercises to strengthen the muscles around your spine, improve flexibility, and reduce pressure on the affected disc. Regular physical therapy sessions can significantly improve your mobility and decrease pain over time.
Functional Disc Stabilization™
At the Illinois Back Institute, we offer a unique approach called Functional Disc Stabilization™. This non-invasive, drug-free treatment focuses on reversing disc degeneration. It uses cycles of compression and traction movements to naturally replenish fluids in the discs. This method has proven success with tens of thousands of patients, providing a healthier and stronger back without the need for medications, surgery, or painful injections.
Why Choose Non-Surgical Options?
Non-surgical treatments allow you to manage your herniated disc symptoms without the risks associated with surgery. They focus on healing and strengthening your body naturally. With the right combination of rest, medication, physical therapy, and innovative treatments like Functional Disc Stabilization™, you can reduce pain and improve your quality of life.
In the next section, we’ll answer some frequently asked questions about herniated discs to help you understand your condition better.
Frequently Asked Questions about Herniated Discs
How do I know if I have herniated my disc?
Diagnosing a herniated disc starts with a visit to your doctor. They will conduct a physical exam, checking your range of motion, reflexes, and muscle strength. You might be asked to perform movements to see what triggers your pain.
If further investigation is needed, your doctor may recommend imaging tests like an MRI or a CT scan. These tests provide detailed images of your spine, helping to pinpoint the herniated disc and assess its impact on nearby nerves.
Can a herniated disc heal on its own?
Yes, a herniated disc can often heal with rest, time, and conservative care. Most people see improvement within a few weeks to months. It’s crucial to avoid activities that worsen the pain and to follow a plan that includes gentle exercises and possibly physical therapy.
Over-the-counter anti-inflammatory drugs can help manage pain and reduce inflammation. However, if symptoms persist beyond six months, consider consulting a healthcare professional for further guidance.
What are emergency symptoms of a herniated disc?
While most herniated discs improve with conservative treatment, some symptoms require immediate medical attention. Severe pain that doesn’t improve, sudden loss of sensation, or weakness in your limbs could indicate a more serious issue.
Bladder or bowel dysfunction, such as incontinence, is a red flag for a condition known as Cauda Equina Syndrome. This is a rare but serious condition where the herniated disc compresses the spinal canal’s nerves. If you experience these symptoms, seek emergency medical care immediately.
Understanding these aspects of herniated discs can help you take the right steps towards recovery. In the next section, we’ll explore more about the benefits of non-surgical treatments and how they can aid in your healing journey.
Conclusion
At the Illinois Back Institute, we understand how debilitating a herniated disc can be. Our focus is on providing natural pain relief through non-surgical treatments. We believe in helping our patients regain their quality of life without the need for invasive procedures or drugs.
Our signature approach, Functional Disc Stabilization™, is a non-invasive, non-surgical, and drug-free treatment option. It has proven success with tens of thousands of patients. This method works by reversing disc degeneration, which leads to a healthier and stronger back. Our goal is to help you avoid the discomfort and risks associated with surgery or painful injections.
If you’re dealing with a herniated disc, know that you have options. Many people find relief through conservative care, and surgery is rarely necessary. With the right approach, you can manage your symptoms and return to normal activities.
For those interested in exploring non-surgical treatment options, we encourage you to learn more about Functional Disc Stabilization™. Our team is dedicated to supporting you on your journey to recovery, ensuring you receive the best care custom to your needs.
You don’t have to live with the pain. With our help, you can find a path to relief and get back to enjoying life. Contact the Illinois Back Institute today for your FREE CONSULTATION to start your journey toward a pain-free life.